In the past few decades, we’ve become increasingly aware of the fact that emotional stress can have a very potent physical effect.
Combined with the most stressful year in a century thanks to the coronavirus pandemic, economic downturn, travel restrictions, and more complications all on top of the usual stressors of life, it’s perfectly natural to take stock of your overall stress level and how it’s affecting you.
In this article, we’ll explore one particular area of concern — stress’s relationship with diabetes — and discuss how now and after the COVID pandemic, you can take a few key steps to prevent stress from affecting your physical and mental health.
First, What Causes Diabetes?
According to the American Diabetes Association, diabetes mellitus is classified as a chronic difficulty with hyperglycemia (high blood glucose), which can be caused by two different underlying conditions.
In type 1 diabetes, hyperglycemia is caused by an autoimmune condition in which your immune system mistakenly attacks the beta cells that produce insulin.
It’s still not entirely understood what causes type 1 diabetes, and as of the time of publishing this article, there is no known cure.
In type 2 diabetes, high blood glucose is caused by insulin resistance, a condition caused by the accumulation of excess dietary fat in cells that aren’t designed to store large quantities of fat, which in turn inhibits the action of insulin.
Type 2 diabetes is correlated heavily to lifestyle and diet with some consistent risk factors like:
Below, we’ll explore how stress affects your blood glucose, as well as how the side effects of stress (which can include many of the risk factors above), can help lead to prediabetes and type 2 diabetes.
Does Emotional Stress Affect Blood Glucose Levels?

Studies are relatively clear on the fact emotional stress raises your blood glucose in the short term.
This happens because elevated emotional stress levels can elicit a biological fight-or-flight response. Then, your body releases cortisol (stress hormones) that increases your blood glucose so that you have energy available to survive.
In the case of chronic stress, this process happens again and again, which can be very damaging for both your mental health and your immune system.
Can Stress Cause High Blood Sugar Levels In Non-Diabetics?
Yes, most healthcare professionals agree that this initial stress response is universal to both people with diabetes and without.
This also includes the long term effects of chronic stress, like a strained immune system, and glucose control.
However, for individuals who already have difficulty keeping their blood glucose low due to diabetes, these spikes in blood glucose can be more pressing and dangerous.
Can Stress Cause Prediabetes or Type 2 Diabetes?
Saying that stress (or its alternatives like burnout) causes prediabetes or type 2 diabetes isn’t entirely accurate.
What is more accurate is that the physical response to stress, as well as the habits that are often associated with stress, all contribute to a higher risk for type 2 diabetes.
On the physical side, recent research has shown that oxidative stress and chronic inflammation — two common side effects of chronic emotional stress — can directly increase insulin resistance and inhibit beta cell function.
As these are the two direct contributors to the development of type 2 diabetes, this is a relatively direct link between stress and diabetes risk factors.
On the mental side, many of the behaviors that are commonplace in stressed individuals — comfort eating, not exercising as much as they’d like, poor sleep, elevated consumption of drugs and alcohol, weight gain, and a poor diet — are all risk factors for type 2 diabetes.
In this way, not only does stress directly increase your risk of type 2 diabetes through physical responses, but it’s likely that many of the habits you might resort to during times of stress may also contribute to the development of type 2 diabetes.
Can Stress Cause Gestational Diabetes?
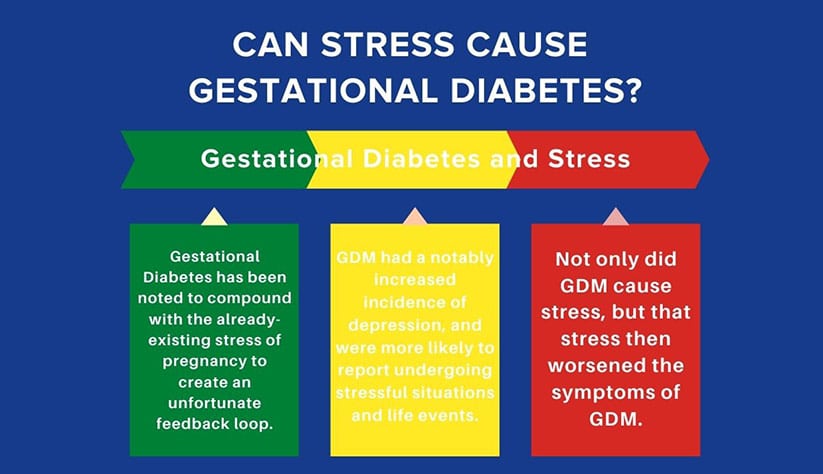
Gestational Diabetes Mellitus (GDM) is a pregnancy-related form of diabetes that can occur suddenly during pregnancy.
Its risk factors are similar to other forms of diabetes, including a previous history or family history with the disease, problems with diet and exercise, poor sleep, obesity, or preexisting high blood glucose.
However, gestational diabetes has been noted to compound with the already-existing stress of pregnancy to create an unfortunate feedback loop.
For example, one study found that women diagnosed with GDM had a notably increased incidence of depression, and were more likely to report undergoing stressful situations and life events. So GDM — its diagnosis, management, and physical toll — leads to more stress.
In addition, other studies found that high levels of stress also raised blood glucose considerably in people with GDM. So not only did GDM cause stress, but that stress then worsened the symptoms of GDM.
If you’re concerned about your stress levels or overall health, it might be worth reaching out to your doctor if you’re thinking about getting pregnant, to help prepare yourself as best as possible for pregnancy.
However, in the case that you’re dealing with an unplanned pregnancy, or currently dealing with GDM, the good news is that some small changes can turn this negative GDM feedback loop into a positive one.
This is because many of the behaviors that reduce stress can also reduce your risk of GDM and type 2 diabetes, and also help combat insulin resistance.
Be sure to read our definitive guide to gestational diabetes to get a comprehensive overview of how to prevent and reverse it.
Concerned That Stress Is Affecting Your Well-Being?

As we saw with GDM, the combination of stress and diabetes (or any form of poor health) can be a negative feedback loop. When your physical and behavioral response to stress helps cause diabetes, which causes more stress, it’s easy to feel helpless.
Fortunately, it just takes one small shift in gears to make a big change. This is because many of the same habits that can help provide long-term relief from stress also help reduce insulin resistance (the complication of type 2 diabetes and GDM) and increase your overall health.
Exercise is one excellent example. A low-fat, plant-based, whole food diet that’s high in whole carbohydrates is another. Losing weight through dietary plans like intermittent fasting is a third.
This is without even adding tactics like getting enough sleep, finding time to relax, spending more time outdoors, and many other strategies that have been proven to help control and reduce stress.
If you’re currently struggling with stress and diabetes, you might be able to learn from the Mastering Diabetes Method, which is proven to reverse insulin resistance and improve your physical health in the long term.
With this method and the guidance and support of our coaches, if you’d like it, you can work on the physical side of stress, and ensure that your body and brain are as healthy as they can be.
Beyond Physical: Stress Management
We also want to acknowledge that there are many aspects of stress beyond just the physical.
Our team members are experts in diabetes care and diabetes management, but stress is a complicated part of life, and a fundamental part of it is mental and emotional.
No matter how physically healthy you are, no matter how successful, no matter where you come from or what your age, it’s still possible to feel too stressed.
And while there are strategies for stress reduction and stress management that we can recommend — like eating healthier, making time for physical activity — sometimes your wellbeing needs a little more assistance.
In these cases, we recommend reaching out to a family member, a mental health professional, or your doctor for some guidance as to a treatment plan to help overcome stress.
Because the research shows that when it comes to your overall health (especially if you’re living with diabetes) improving your stress management can sometimes be just as helpful as medical advice.
Stop Guessing What to Eat
Get Delicious Recipes Sent to Your Inbox Every Week!
Discover the custom-designed Weekly Meal Plan that gives you clarity on what to eat and how to shop to simplify your journey to lower blood sugar, weight loss, and your best A1c