What is Type 1.5 Diabetes?
Type 1.5 diabetes is the unofficial term for latent autoimmune diabetes in adults, a condition similar to type 1 diabetes where your immune system mistakenly targets the insulin-producing beta cells in your pancreas, slowly (over 5-10 years) diminishing your ability to naturally regulate your blood glucose.
Sometimes referred to as late-onset type 1 diabetes, this form of diabetes is frequently misdiagnosed as type 2 diabetes (with one report showing 15% of cases were misdiagnosed).
This can be frustrating and confusing, especially to those carefully planning their diet and exercise to combat type 2 diabetes, but seeing poor results through no fault of their own.
In this article, we’ll focus on how type 1.5 diabetes is unique. We’ll talk about differences between type 1.5 diabetes and other similar forms (type 1 and type 2 diabetes), as well as genetic risk factors and common symptoms.
We’ll also focus on the C-Peptide test, a fundamental test for determining your type of diabetes accurately, and how to effectively manage this autoimmune condition.
How Does Type 1.5 Differ From Type 1 Or Type 2 Diabetes?
The onset of type 1.5 diabetes occurs much slower and later in life than that of type 1 diabetes. Also, the root causes of type 1.5 diabetes and type 2 diabetes are very different.
Like type 1 diabetes, type 1.5 diabetes is an autoimmune condition in which your immune system mistakenly creates autoantibodies, which attack the beta cells and other enzymes like Glutamic Acid Decarboxylase (GAD) on the beta cells in your pancreas.
However, unlike type 1 diabetes, type 1.5 diabetes has a slow onset and typically occurs in your 30s, rather than in childhood or adolescence.
This adult-onset, slow-progressing form of diabetes has a similar symptomology to type 2 diabetes, and because of this, type 1.5 diabetes is often misdiagnosed as type 2 diabetes.
However, type 2 diabetes is fundamentally different from type 1.5 diabetes because it is caused by insulin resistance and is not an autoimmune condition.
Is Type 1.5 Diabetes Hereditary?
Researchers are currently unclear on the exact factors that trigger type 1.5 diabetes.
However, there is evidence-based research that shows that there is a clear genetic component to the disease. A family history of type 1.5 diabetes is a strong risk factor, but despite this, researchers are still searching to understand exactly how the disease can be inherited.
Type 1.5 Diabetes Prevention
Like type 1 diabetes, there is currently no research that consistently shows how type 1.5 diabetes can be prevented. However, certain individuals are more likely to develop type 1.5 diabetes than others.
In the case of type 1.5 diabetes, the best prevention is preparation. Whether this type of diabetes onsets or not, the goal is to keep your body insulin sensitive for as long as possible.
This is best done by avoiding conditions like prediabetes, keeping an ideal BMI, and calibrating your diet and lifestyle for insulin sensitivity. In this way, if you do develop type 1.5 diabetes, you are already in ideal health, and able to immediately control your blood glucose and insulin use easily.
With proper diet and lifestyle strategies, type 1.5 diabetes is a chronic condition that can be effectively and easily managed.

Symptoms of Type 1.5 Diabetes
All of the initial symptoms of different types of diabetes are very similar, caused by sustained high blood glucose (hyperglycemia).
These initial symptoms include:

In the Case of Type 2 Misdiagnosis

One of the main problems with type 1.5 diabetes is that it can often be misdiagnosed as type 2 diabetes. Unfortunately, this happens in the overwhelming majority of all cases, often resulting in an improper treatment method for extended periods of time.
In this case, a secondary set of symptoms may occur. These symptoms include:
How is Type 1.5 Diabetes Diagnosed?
When addressed properly, type 1.5 diabetes is diagnosed in two phases.
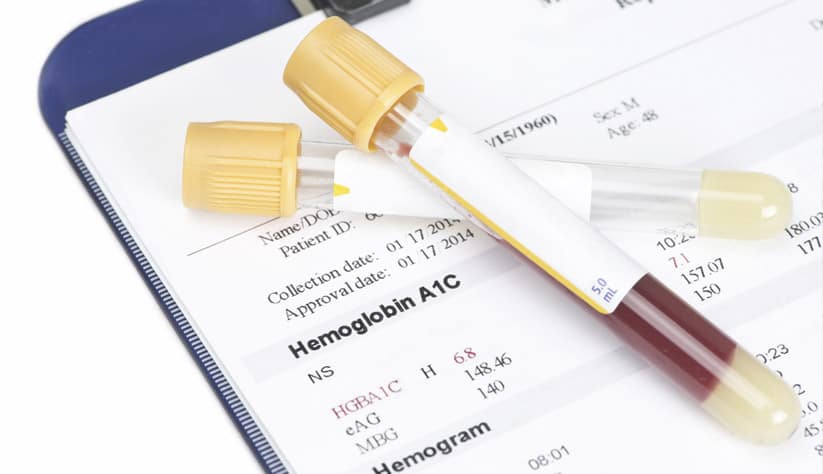
First, you’ll take either an oral glucose tolerance test (OGTT) or an HbA1c test (commonly known as the A1c test). Both diagnostic tests are used to identify if your body can sufficiently metabolize glucose.
In adult-onset forms of diabetes, many healthcare professionals improperly diagnose an elevated A1c value, fasting glucose, and/or poor performance on an OGTT as type 2 diabetes.
However, to fully determine whether you may be living with type 1.5 diabetes, you’ll require two additional tests:
- A C-peptide test which determines your body’s ability to produce endogenous (self-made) insulin
- A diabetes antibody panel which determines whether you test positive for one or multiple antibodies that affect insulin production
Long-Term Complications of Type 1.5 Diabetes
If left untreated, type 1.5 diabetes can lead to complications including kidney disease and diabetic ketoacidosis (DKA).
If left untreated for long enough, it can also result in the development of insulin resistance, which is referred to as “double diabetes.”
Double diabetes can result in heart disease, cardiovascular disease, high blood pressure, and increase your risk for many conditions.
Can Type 1.5 Diabetes be Reversed?
Though much research is currently being done on type 1 and type 1.5 diabetes, at the moment these autoimmune diseases have no known cure.
However, type 1 and type 1.5 diabetes can be effectively and precisely managed, and the risks of these conditions are minimized through the use of exogenous insulin, as well as through diet and lifestyle changes.
How to Treat Type 1.5 Diabetes
There are two main parts of the long term treatment type 1.5 diabetes. The first part is the use of exogenous (external) insulin, which makes up for the insulin that the beta cells in your pancreas no longer secretes
The second part is smart diet and lifestyle choices, which can drastically improve your insulin sensitivity. Increased insulin sensitivity is fundamental to treatment for all forms of diabetes, and results in many improvements, as we have documented in our own research:
Lifestyle Changes | The Right Diet and Daily Movement
Three very simple, very powerful lifestyle changes can drastically improve your health with type 1.5 diabetes.
The Low-Fat, Plant-Based, Whole-Food Diet — This evidence-based diet is tailor-made to improve your insulin sensitivity in the long run, without the negative effects of some other alternatives. No portion restrictions are needed!
Daily Movement — The research is clear: daily movement helps improve insulin sensitivity. Finding an activity that you look forward to doing can drastically increase your health in the long run.
Intermittent Fasting — Using your body’s natural process for recycling old cells, damaged proteins, and accumulated triglycerides that can dramatically lower your weight, reduce insulin resistance, reduce oxidative stress, and vastly improve your immunity.
Intermittent Fasting — Using your body’s natural process for recycling old cells, damaged proteins, and accumulated triglycerides that can dramatically lower your weight, reduce insulin resistance, reduce oxidative stress, and vastly improve your immunity.

Managing Type 1.5 Diabetes Using Medication

Insulin therapy — supplementing your body with exogenous insulin through a pen, syringe, or pump — is fundamental to managing type 1.5 diabetes, and becomes a part of the daily routine.
However, oral medications like metformin and sulfonylureas often don't work for managing type 1.5 diabetes because they don't solve the underlying problem of insulin deficiency.
In the early stages, it may be necessary to take diabetes medications to help stabilize your blood glucose. However, these can have negative side effects, and the end goal is to reduce or eliminate oral medications, and instead manage type 1.5 diabetes with insulin and your lifestyle.
Managing Type 1.5 Diabetes Using Medication
For guidance on other forms of diabetes, you can see our articles on:
Get Support
No matter what form of diabetes you have, the good news is that you can control it and manage it with your diet and lifestyle.
The most important step is to fully understand which form of diabetes you have, so you can plan treatment effectively.
Fortunately, the same methods for prevention and treatment are all exactly the same, so you can form and maintain the same habits, and find a community of others doing the same, no matter which form of diabetes you may have.
However, we understand that some of these habits can be a big change, which is why we have a team of diabetes care experts here to support you.
Register for the masterclass below to discover how the Mastering Diabetes Method can truly transform your diabetes health living with type 1.5 diabetes.
Stop Guessing What to Eat
Get Delicious Recipes Sent to Your Inbox Every Week!
Discover the custom-designed Weekly Meal Plan that gives you clarity on what to eat and how to shop to simplify your journey to lower blood sugar, weight loss, and your best A1c